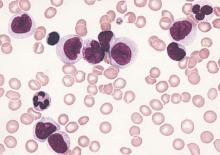
Clinical outcomes were significantly worse among younger patients with secondary and therapy-related acute myeloid leukemia (sAML and tAML, respectively) compared with de novo disease, suggesting the presence of distinct AML subtypes, in a study published online Aug. 24 in Journal of Clinical Oncology.
In the Danish population-based study, patients under age 60 with de novo AML had a 3-year survival rate of 52%, compared with 35% for AML secondary to myelodysplastic syndrome (MDS-sAML), 19% for AML secondary to chronic myelomonocytic leukemia or myeloproliferative neoplasia (non-MDS-sAML), and 27% for tAML.
Non-MDS-sAML was associated with poorer outcomes at any age, but patients older than 60 years with MDS-sAML and tAML had outcomes similar to those of de novo AML, Dr. Lene Sofie Granfeldt Ostgard and associates reported (J Clin Oncol. 2015 Aug 24. doi:10.1200/JCO.2014.60.0890).
The cohort study evaluated records of 3,055 patients diagnosed with AML from 2000 to 2013. Overall, 73.6% had de novo AML, 19.8% had sAML (11.5% MDS, 8.3% non-MDS), and 6.6% had tAML. The researchers focused on the 1,567 patients (51.3%) who underwent curative intent therapy. Patients with sAML were less likely to receive intensive therapy than were patients with tAML or de novo AML. Patients who underwent intensive treatment had superior survival rates compared with patients within the same subgroup who did not undergo treatment.
Contrary to previous reports, the investigators did not observe an increase in the incidence of AML, sAML, or tAML over the 14-year study period. They did, however, find that clinical trial accrual rates for patients with sAML and tAML increased significantly over that period, which may account for reports of a temporal increase in tAML.
Adverse-risk cytogenetics were most prevalent in patients with tAML, likely because of clonal selection of chemotherapy-resistant p53-mutated cells. Patients with non-MDS-sAML had a higher frequency of aberrant karyotypes, though not classified as adverse, which the authors speculate may explain the worse outcomes observed in this group.
“Given the extremely poor prognosis associated with an antecedent diagnosis of CMML [chronic myelomonocytic leukemia] or MPN [myeloproliferative neoplasia], these entities should be considered separately from prior MDS when investigating outcomes and new treatment strategies in patients with sAML,” wrote Dr. Ostgard of Aarhus University Hospital, Denmark, and colleagues.
The presence of MDS-sAML and tAML was associated with worse survival, but the association was weaker in older patients and those with adverse cytogenetics, suggesting the relative effect of MDS or prior chemotherapy is small in patients with an already poor prognosis.
Dr. Ostgard reported consulting or advisory roles with Bristol-Myers Squibb and Abbvie. Several of her coauthors reported ties to industry sources.