Women who are overweight and obese have a significantly higher risk of invasive breast cancer after menopause compared with normal-weight women, according to secondary analysis of data from the Women’s Health Initiative.
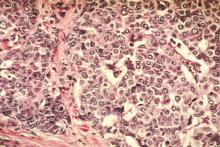
An analysis of data from 67,142 postmenopausal women aged 50-79 years found that women with a body mass index greater than 35 had a 58% increased risk of invasive breast cancer, compared with women with a BMI lower than 25. Obese women with a BMI of greater than 35 were also at increased risk for estrogen- and progesterone-receptor–positive breast cancer compared to normal-weight women (hazard ratio, 1.86), but they were not at increased risk for hormone receptor–negative breast cancer.
This group also had a twofold increase in the risk of being diagnosed with a larger tumor, and significantly higher risk of having positive lymph nodes, regional and/or distant stage, and also of dying after breast cancer, according to an article published June 11 in JAMA Oncology.
“Well-designed clinical trials are needed to definitively test whether weight loss and body composition changes in overweight and obese women or obesity prevention in women of normal weight will reduce breast cancer risk,” wrote Marian L. Neuhouser, Ph.D., of the Fred Hutchinson Cancer Research Center in Seattle, and her colleagues (JAMA Oncol. 2015. June 11 [doi: 10.1001/jamaoncol. 2015.1546]).
The Women’s Health Initiative programs are supported by the National Heart, Lung, and Blood Institute, part of the National Institutes of Health. One of the researchers disclosed having financial relationships with Novartis, Novo Nordisk, Pfizer, Genetech, and Amgen. The other researchers reported having no financial disclosures.